Biden’s Healthcare Problem
Biden’s Healthcare Problem
Deeply ingrained inequalities—many of which are reflective of the country’s patchwork healthcare system—belie rosy projections that Biden is delivering inclusive growth.
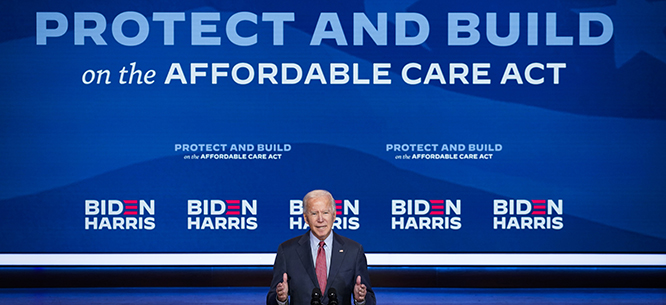
Since the Affordable Care Act passed in 2010, there has been crucial—if labored—progress toward de facto universal healthcare in the United States. According to the U.S. Census Bureau, the number of non-elderly uninsured people declined from roughly 48 million in 2010 to 25.6 million in 2022. At this peak, 92 percent of the U.S. population, or about 304 million people, had some form of health insurance.
These promising numbers, however, faced a difficult setback last year thanks to the “unwinding” of emergency Medicaid coverage established during the pandemic. Backed by additional federal funding, the Families First Coronavirus Response Act included a “continuous enrollment provision” that extended coverage to millions of workers who lost employment at the start of the pandemic. This temporary federal expansion of Medicaid, which helped raise enrollment by over 21 million people, was among the most important interventions of the emergency welfare state constructed between the Families First Act and the 2021 American Rescue Plan Act. But since emergency extensions expired in March 2023 under the Consolidated Appropriations Act, 19.6 million people have lost Medicaid, according to the healthcare policy research nonprofit KFF.
While some of those who were kicked off Medicaid have subsequently qualified for a partly subsidized ACA marketplace plan, there is a high probability that many will fall through the cracks and remain uninsured. According to a January 2024 report from the Centers for Medicare & Medicaid Services, only 2.4 million of the 21.3 million enrollments in the ACA marketplace in 2023 were people who previously had Medicaid or CHIP (Children’s Health Insurance Program). With disenrollment numbers continuing to rise, there is little doubt that the “coverage gap” will widen among lower-income households—particularly those in states with the worst overall health system performance (the majority of which are in the South and dominated by Republicans).
This gap exists for penurious reasons but also because the United States’ public-private health system is maddeningly complicated. In states with stringent Medicaid eligibility rules, many low-income people lack health insurance because their incomes are too high for Medicaid but too low to qualify for ACA subsidies. But too many people remain uninsured even in the bluest states; in 2022, only Massachusetts, Hawaii, and Iowa had an uninsured population below 5 percent. Those who have recently lost Medicaid for procedural reasons or no longer qualify due to relatively modest increases in income are likely to be overwhelmed by the prospect of new healthcare expenses. With the exception of New York and Minnesota, even the least expensive ACA plans cost more than Medicaid, which includes a number of mandatory, fully subsidized benefits and mostly nominal fees for out-of-pocket expenses. Those who have not transitioned to a marketplace plan may be deterred by higher costs, including monthly premiums, deductibles, co-payments, and fees for prescriptions and other services.
Above all, families with young children are the most vulnerable. During the height of the pandemic, new mothers were among the most important beneficiaries of continuous enrollment. The number of uninsured children, meanwhile, dropped to 3.9 million in 2022, down from 4.4 million in 2019—a significant improvement given the steady increase under the Trump administration. Black families and other minorities who have historically experienced disparities in healthcare also benefited. But policy experts warn that progress is reversing. As of April 2024, at least 3,400,000 children have been disenrolled from Medicaid, while minority groups are projected to disproportionately comprise those who fall into the longer-term gap. At the same time, additional subsidies for the ACA marketplace included in the Inflation Reduction Act are slated to expire at the end of 2025; the Urban Institute has estimated that another 3 million people will lose insurance if they are not renewed.
As we head toward the 2024 election, influential liberal commentators are hailing the country’s remarkable rebound from the pandemic recession and arguing that the economy is the strongest it’s been in decades. Yet deeply ingrained inequalities—many of which are reflective of the country’s patchwork healthcare system—belie rosy projections that Biden is delivering inclusive growth. On top of the affordable housing crisis, more expensive groceries and utilities, and rising interest rates for credit cards and auto insurance, higher healthcare costs exacerbate the pervasive sense that the cost of living is out of control.
In addition to increased costs, changes to how healthcare is delivered impose a distinct psychological burden on working-class Americans who don’t have spare time to navigate a cumbersome system, compare policies, and calculate a new healthcare budget. Research indicates that, depending on the program, between 20 and 75 percent of households eligible for welfare programs do not use them due to bureaucratic hurdles, compliance costs, and social stigma. Between those families and individuals who struggle to obtain new coverage and those discouraged by the quality and costs of their new plans, many working Americans now have another reason to doubt Democrats’ promises about the economy.
Before it was fully implemented, the ACA appeared to be an albatross undermining Democratic fortunes. Following the anti-government Tea Party insurgency, public wariness about the landmark healthcare reform ran high. An avalanche of propaganda about “death panels”—the false accusation made by Sarah Palin and others on the right that government-subsidized healthcare would deny services to the elderly and those with disabilities—contributed to Republicans winning a House majority in the 2010 midterms. In fact, it was only after the Trump administration’s bungled attempts to repeal the ACA that polling revealed a clear majority of Americans supported the law.
A key reason the ACA is popular is because it prohibits insurance companies from denying coverage to those with preexisting medical conditions. But the crown jewel of the law is the expansion of Medicaid, the Great Society program that has provided federal- and state-funded medical care to the poorest Americans since 1965. Forty states and the District of Columbia have adopted the Medicaid expansion, which raised the income threshold for non-elderly adults to 138 percent of the federal poverty level.
The expansion hasn’t reached everybody. In 2012, the Supreme Court ruled that the ACA’s Medicaid mandate was unconstitutional, which allowed the most conservative state governments to opt out and keep Medicaid eligibility at or below the poverty line.
And yet despite the fact that populous states such as Texas and Florida continue to reject expansion, steady gains have been made toward shrinking the coverage gap: in March 2023, over 86.7 million individuals were enrolled in Medicaid, an increase of around 32 million people since 2010, when the depths of the Great Recession and foreclosure crisis had added more than 6 million to Medicaid rolls. In the states that opted into the expansion, the 2024 threshold for a family of four to qualify for Medicaid is $43,000 a year. For those families, the ACA has been a fulcrum of basic fairness in an era of protracted wage stagnation and soaring housing costs.
Much of the growth in Medicaid coverage from 2020 to early 2023 can be attributed to the continuous enrollment provision, which raised enrollment in every state regardless of whether they had adopted the ACA’s Medicaid expansion. By preventing individual states from disenrolling people from Medicaid for the duration of the pandemic, the continuous enrollment measure effectively paused ACA income reviews for the program’s recipients from February 2020 to March 2023. This allowed some households whose income increased to continue receiving fully subsidized healthcare for longer than they otherwise would have. That dynamic partly accounts for the flux in coverage and the confusion over insurance options over the last year: among the bottom quarter of households, there has been wage growth of between 3 and 9 percent over the last four years, moving some families above the threshold for Medicaid eligibility.
The surge in people losing healthcare has been exacerbated by several avoidable problems. While policy experts are still collecting data on the millions of households that have not since obtained an ACA plan, they include a few categories: people who were unaware of the “unwinding” and don’t know about the Biden administration’s extended enrollment window for the ACA marketplace; people whose income now disqualifies them from re-enrollment in Medicaid but who cannot afford the total costs of an ACA plan or do not know about the expanded ACA tax credits; people wrongly disqualified from Medicaid who lack the time or ability to dispute the outcome; people in Republican-dominated states such as Texas, which have reverted back to stricter eligibility requirements; and people whose personal circumstances have made it otherwise difficult to adapt to the policy change.
The growing gap has been compounded by state-level administrative errors, but it also stems from Congress’s unrealistic outlook. It seems that many in Washington expected the “unwinding,” announced through official marketplace notices, would lead to a direct transition to either employer-provided insurance or a low-cost ACA plan. Provided the former was unavailable, people could access HealthCare.gov or contact their state’s marketplace exchange and update their household information in order to obtain insurance, much as other ACA customers did. In theory, the tax credits that came with the Inflation Reduction Act, known as advance premium tax credits (APTC), would contain any growth in the coverage gap since they kick in at 100 percent of the federal poverty level. Individuals and families who moved out of poverty during the pandemic, Democrats hoped, would switch to a marketplace plan with minimal inconvenience or financial burden.
The best intentions, however, cannot mask a simple fact of the U.S. healthcare system: it remains needlessly complex for the average consumer. The fact that the coverage gap exists even in states that have fully adopted the ACA and tried to further improve healthcare access shows that there are too many obstacles to adequate care. The ACA, with its complex and evolving parameters, tasks more time-strapped households, particularly those headed by adults without a college degree, with understanding and managing their “care options.” Even programs like the APTC, meant to directly benefit households buying insurance, are confusing and difficult to use: consumers must know what the APTC is, know how to access it on the marketplace platform, and gauge how they can most benefit from it. (The APTC can also be clawed back in the form of tax penalties if a household’s annual income is higher than it was projected to be at the time of enrollment.)
Another problem is how ill-suited the ACA marketplace is for workers in sectors that don’t offer reliable hours and wages. For millions of workers, many of whom are earning under $20 per hour, wages change month-to-month and year-to-year. And to the extent they are a real phenomenon, rising wages are concentrated in service subsectors like restaurant and retail. The ACA requires annual tax filings to determine coverage and—at least in theory—immediate notification of any change in income. A barista, cook, or sales clerk may strategize to slightly increase their income, not factoring that some of the fruits of their labor may be absorbed by higher health insurance costs.
That says nothing about how affordable treatment is for those who do have insurance. The APTC, for instance, doesn’t apply to co-pays and deductibles, which are usually higher for lower-cost plans. Moreover, many households defer treatments and screenings for health problems, even when they are paying for upper-tier plans, because of growing uncertainty about what final bills will be for both routine doctor’s visits and more serious medical interventions. According to Gallup, almost 40 percent of Americans reported that they or a family member put off medical treatment in 2022, a record high since polling on the question began in 2001. Cost-driven delays in medical treatment have made Americans sicker and lowered their life expectancy.
As Democrats bitterly learned in the Carter era—the last time inflation and interest rates simultaneously surged—lower-income workers are usually quite price-sensitive and disproportionately feel the weight of moderately higher bills. They are likewise alert to new ones—something that is happening to many working families who have obtained a marketplace plan since losing Medicaid. The ambiguities and trade-offs that low-income households must navigate to acquire and use insurance illustrate the disjuncture between what the ACA has achieved on paper and how people experience the country’s sprawling public-private healthcare system.
According to a March 2022 KFF poll, only 20 percent of those who said the ACA had helped them reported that it had lowered their healthcare expenses. Individual consumer assessments may not always be accurate, as recently evidenced by the lack of knowledge of new limits on prescription drug prices under Medicare. But ten years on from the ACA’s implementation, it’s clear that the law’s architects failed to anticipate the problem of expensive and rising deductibles. Without regulatory interventions that go beyond patchwork remedies like tax credits, ACA enrollees will remain subject to unpredictable and unmanageable costs.
ACA costs continue to inch upward despite government subsidies, and insurers have warned that inflationary pressures are expected to mount throughout the healthcare sector in 2024. That development could interfere with the post-pandemic economic “soft landing”—the pursuit of steady disinflation without triggering a recession—that the Federal Reserve and the Biden administration have attempted to engineer. The expiration of emergency Medicaid, combined with rising premiums, co-pays, and deductibles, could depress consumer spending among the workers and demographics whom Biden has promised to lift up, slowing economic growth just as the 2024 campaign hits full swing.
Democrats might privately reason that Medicaid disenrollment is not a serious electoral liability at the national level, on the basis that poor people don’t vote in large numbers or with any regularity. Yet current net disenrollment figures from individual states suggest such reasoning could be politically fallacious. In addition to Georgia, the crucial swing states of Pennsylvania, Michigan, Arizona, and Wisconsin have all seen steep drops in Medicaid coverage. Given that Donald Trump will likely have an edge in the Electoral College, any one of those states could make or break Biden’s reelection. Indeed, just as infrastructure projects and new manufacturing jobs could add a few thousand voters to Biden’s coalition, so too could disaffection over inflation and lost healthcare lead thousands of irregular working-class voters to stay home on election day—or cast a protest vote.
In the absence of any immediate policy fixes, Democrats will have to become more tactful in how they discuss healthcare on the campaign trail. But this does not mean shrinking from a vision of what they aim to achieve: health policy remains the central way the welfare state can be harnessed to dramatically improve developmental outcomes, spread economic opportunity, and contain household bills. If they want a second Biden administration, Democrats must offer concrete plans to alleviate the health-related financial woes that too many families shoulder, including medical debt that burdens over 100 million Americans. They should also highlight how the administration’s burgeoning antitrust agenda is already leading to reforms that save Americans from predatory practices, like the No Surprises Act, which aims to prevent unexpected medical bills.
Millions of Americans still face profound obstacles to acquiring reliable, uninterrupted, and affordable healthcare. This is a consequence not merely of conservative obstructionism but of Democrats’ patchwork approach to the issue. While most working Americans now have a tangle of options to obtain basic care, they have few assurances overall costs won’t continue to rise, regardless of the ebb and flow of real wage gains. If the Democratic Party cannot resolve to arrest another surge in regional, racial, and income-based health disparities, the inequalities that characterized the neoliberal era will only persist.
Justin H. Vassallo is a writer specializing in American political development, political economy, party systems, and ideology, and a columnist at Compact magazine.